|
Description
|
Image
|
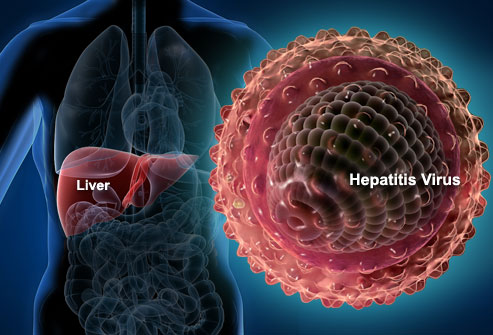
01. What Is Hepatitis?
Hepatitis is an inflammation of the liver. It may be caused by drugs, alcohol use, or certain medical conditions. But in most cases, itís caused by a virus that infects the liver. This is known as viral hepatitis, and the most common forms are hepatitis A, B, and C.
|
|
02. Hepatitis Symptoms
Sometimes there are no symptoms of hepatitis in the first weeks after infection Ė the acute phase. But when they occur, the symptoms of hepatitis A, B, and C may include fatigue, nausea, poor appetite, belly pain, a mild fever, or yellow skin or eyes (jaundice.) When hepatitis B and C become chronic, they may cause no symptoms for years. By the time there are any warning signs, the liver may already be damaged.
|

|
03. Hepatitis A: What Happens
Hepatitis A is highly contagious and can spread from person to person in many different settings. It typically causes only a mild illness, and many people who are infected may never realize they are sick at all. The virus almost always goes away on its own and does not cause long-term liver damage.
|

|
04. Hepatitis A: How Does It Spread?
Hepatitis A usually spreads through contaminated food or water. Food can be tainted when itís touched by an infected person who did not wash his hands after using the bathroom. This transfers tiny amounts of infected stool to the food. Raw shellfish, fruits, vegetables, and undercooked foods are common culprits in hepatitis A outbreaks. The virus can also spread in daycare centers if employees arenít careful about washing hands after changing diapers.
|

|
05. Hepatitis A: Who Is at Risk?
A prime risk factor for hepatitis A is traveling to or living in a country with high infection rates. You can check the CDCís travel advisories to learn about recent outbreaks. Eating raw foods or drinking tap water can increase your risk while traveling. Children who attend daycare centers also have a higher risk of getting hepatitis A.
|

|
06. Hepatitis B: What Happens
Many adults who get hepatitis B have mild symptoms for a short time and then get better on their own. But some people are not able to clear the hepatitis B virus from the body, which causes a long-term infection. Nearly 90 percent of infants who get the virus will carry it with them for life. Over time, chronic hepatitis B can lead to serious problems such as liver damage, liver failure, and liver cancer.
|

|
07. Hepatitis B: How Does It Spread?
You can get hepatitis B through contact with the blood or body fluids of an infected person. In the U.S., hepatitis B is most often spread through unprotected sex. Itís also possible to get hepatitis B by sharing an infected personís needles, razors or toothbrush. And an infected mother can pass the virus to her baby during childbirth. Hepatitis B is not spread by hugging, kissing, sharing food or coughing.
|

|
08. Hepatitis B: Who Is at Risk?
Anyone can get hepatitis B, but people who have multiple sex partners or inject illegal drugs have a higher risk. Other risk factors include being a health care worker who is exposed to blood or living with someone who has chronic hepatitis B.
|

|
09. Hepatitis C: What Happens
About 25% of people who get hepatitis C defeat the virus after an acute infection. The rest will carry the virus in their body for the long term. Chronic hepatitis C can cause very serious complications, including liver failure and liver cancer. Fortunately, there are ways to manage the virus and reduce its impact on the liver.
|
|
10. Hepatitis C: How Does It Spread?
Hepatitis C spreads through infected blood. In the U.S., sharing needles or "works" to inject drugs is the most common cause of infection. Getting a tattoo or body piercing with an infected needle is another means of exposure. A mother may pass the virus to her child at birth. In rare cases, unprotected sex spreads hepatitis C, but the risk appears small. Having multiple sex partners, HIV, or rough sex seems to increase risk for spreading hepatitis C
|

|
11. Hepatitis C: Who Is at Risk?
People who have injected illegal drugs at any time, even one time, many years ago, could be walking around with chronic hepatitis C. Because there are often no symptoms, many former drug users may not realize they have the infection. People who received a blood transfusion before 1992 also have an elevated risk. Prior to that year, donated blood was not screened for the hepatitis C virus.
|

|
12. How Is Hepatitis Diagnosed?
Chronic hepatitis can quietly attack the liver for years without causing any symptoms. Unless the infection is diagnosed, monitored, and treated, many of these people will eventually develop serious liver damage. Fortunately, blood tests can determine whether you have viral hepatitis, and if so, which kind.
10. Hepatitis C: How Does It Spread?
|

|
13. Who Should Be Tested for Hepatitis?
Testing is important for anyone with the risk factors weíve mentioned, particularly injection drug users and people who have had multiple sex partners. Health advocates are also urging people of Asian heritage to get tested. Stanford Universityís Asian Liver Center estimates that 1 in 10 Asians living in the U.S. has chronic hepatitis B. Many of them have probably had the virus since birth.
|

|
14. What If You Test Positive?
If you test positive for viral hepatitis, you can take steps to protect the ones you love. For hepatitis A, wash your hands frequently. For hepatitis B and C, avoid sharing your nail clippers, razor, or toothbrush. Make sure everyone in your household gets the hepatitis B vaccine. An important step is to see a specialist to discuss your treatment options.
|

|
15. Treatment: Hepatitis A
Hepatitis A almost always goes away on its own, and no medication is needed. If nausea is a problem, try eating several small meals throughout the day instead of three large ones. Drink water, juice, or sports drinks to stay hydrated. And avoid strenuous exercise until youíre feeling better.
|

|
16. Treatment: Chronic Hepatitis B
The goal of treating chronic hepatitis B is to control the virus and keep it from damaging the liver. This begins with regular monitoring for signs of liver disease. Antiviral medications may help, but not everyone can take them or needs to be on medication. Be sure to discuss the risks and benefits of antiviral therapy with your doctor.
|

|
17. Treatment: Chronic Hepatitis C
The most common treatment for chronic hepatitis C is a combination of antiviral medications called interferon and ribavirin. Interferon is given as a shot and ribavirin is a pill. Studies suggest this combination can cure or control hepatitis C in about half of patients. But it can cause serious side effects. In addition, not everyone needs treatment. Your doctor will explain your options based on how active the virus is.
|

|
18. Monitoring Chronic Hepatitis
Careful monitoring is the cornerstone of managing chronic hepatitis B and C. Your doctor will order regular blood tests to check how well your liver is working. Ultrasounds and CT scans can also reveal signs of liver damage. If the virus is not causing any liver problems, you may not need treatment. But itís important to have regular tests to watch for changes. Complications are easiest to treat when found early.
|

|
19. Complications: Cirrhosis
One of the most common complications of chronic hepatitis is cirrhosis. This is a scarring of the liver that can be detected with a biopsy. Cirrhosis makes it difficult for the liver to do its job and can lead to liver failure, a life-threatening condition. Symptoms include fatigue, nausea, weight loss, and swelling in the belly and legs. In severe cases, patients may experience jaundice and confusion.
|

|
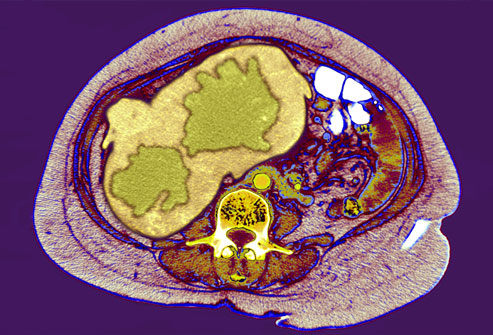
20. Complications: Liver Cancer
Viral hepatitis is the top cause of liver cancer, so people with chronic hepatitis B or C need monitoring even if you feel ďfine.Ē Blood tests can detect proteins that suggest the presence of liver cancer. Ultrasounds, CT scans, and MRIs can reveal abnormal lesions in the liver (seen here in green). A biopsy is needed to determine if these areas are cancerous. Tumors that are found early may be surgically removed. But most liver cancers are difficult to treat.
|
|
21. Liver Transplant
The liver is a vital organ that aids in metabolism, digestion, detoxifying, and the production of many proteins needed by the body. If a large part of the liver is damaged beyond repair, it will no longer be able to perform these important jobs. People cannot live without a working liver. In this case, a liver transplant may be the best hope. This option provides the patient with a healthy liver from a donor.
|
|
22. Hepatitis A and B Vaccines
There are vaccines to protect against hepatitis A and B. The CDC recommends hepatitis A vaccination for all children ages 12 to 23 months and for adults who plan to travel or work in areas with hepatitis A outbreaks. People with chronic hepatitis B or C should also get the hepatitis A vaccine if they donít already have immunity to hepatitis A. The hepatitis B vaccine is recommended for all infants at birth and for adults who have any of the risk factors we discussed earlier. There is no vaccine for hepatitis C.
21. Liver Transplant
|

|
23. Protecting Your Liver
If you have chronic hepatitis, there are steps you can take to keep your liver resilient. Avoid alcohol, which can cause additional liver damage. Check with your doctor before taking any medications or supplements, because some are tough on the liver or may not be safe in people with liver disease. Most importantly, keep your appointments for regular monitoring. By watching for any changes in your liver, you and your health care provider can stay one step ahead of the virus.
|

|